thoracic outlet syndrome and tos: key facts and centre specialize
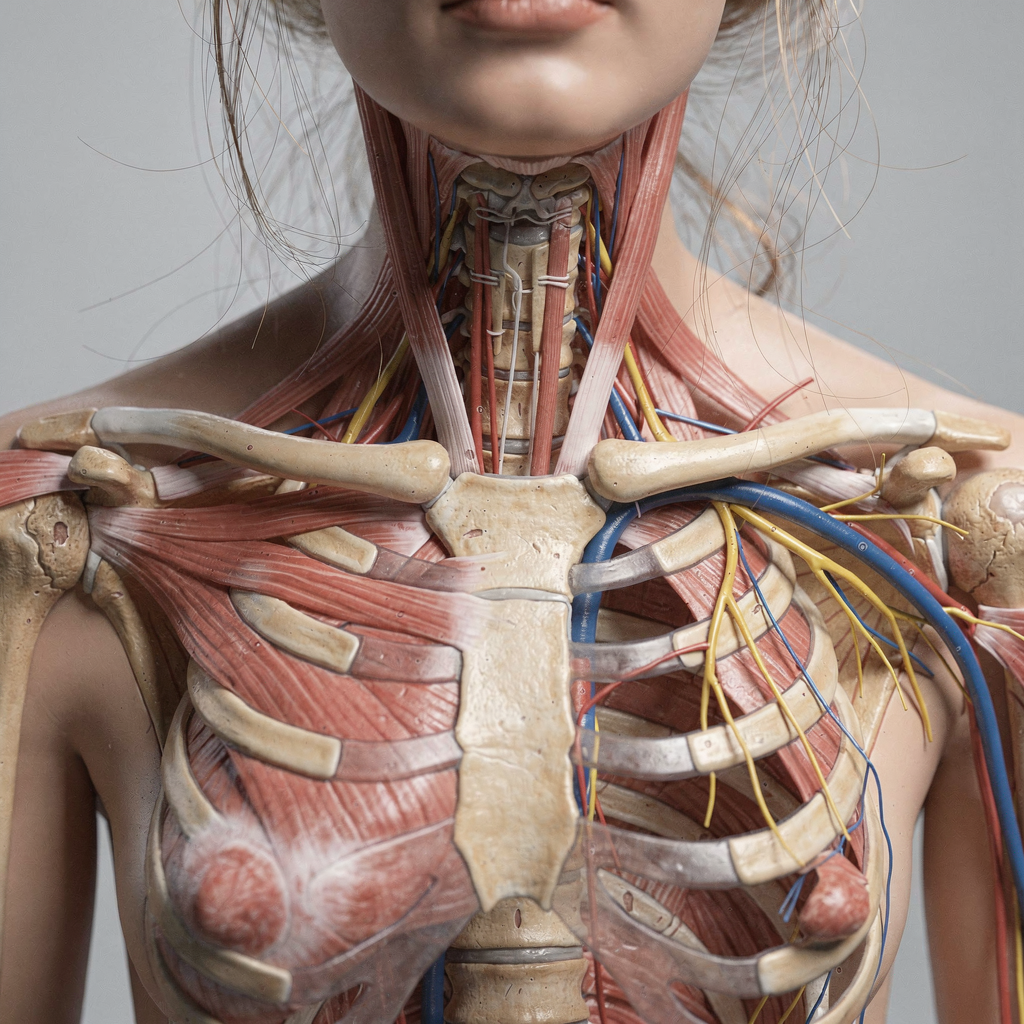
Thoracic outlet syndrome is a condition that affects the space between the collarbone and first rib. It can compress nerves or blood vessels that travel from the neck into the arm. In simple terms, thoracic outlet syndrome refers to a set of symptoms caused by that compression. At our center for thoracic outlet syndrome we combine rapid diagnosis, imaging, and coordinated care. We operate like an academic medical center that streamlines care pathways so patients move from assessment to treatment with fewer delays.
Prevalence varies with age and activity. For example, thoracic outlet syndrome varies by population and often appears in people with repetitive upper chest tasks or overhead work. Repetitive strain can produce neck pain and arm discomfort. Some people are born with an extra cervical rib or an abnormal first rib that narrows the outlet. Others develop symptoms after trauma or prolonged poor posture. The impact on daily life can be substantial. Patients report pain, tingle, numbness, weakness, and limits on work or sports. Conservative care restores function in many patients, and expert care speeds recovery when surgery is needed.
Specialised care improves outcomes because the condition spans several disciplines. We use a multidisciplinary team with vascular surgeons, neurologists, and physiotherapists who work together. We emphasize a comprehensive diagnosis of thoracic outlet syndrome so the team can rule out other conditions that cause similar symptoms. Informed consent and clear communication matter; as one legal review notes, “Terms of Service are the digital contracts of our era,” and patients deserve the same clarity for medical plans “Terms of Service” insight. Also, many users do not read long documents, with over 85% admitting they skip the text, a statistic that underlines the need for plain language in consent forms as reported. Finally, our medical center coordinates diagnostics and treatment so patients receive care that is timely, clear, and evidence-based.
types of thoracic outlet syndrome: neurogenic, venous and arterial
The types of thoracic outlet syndrome divide by what tissue a patient compresses. The common type involves the nerve bundle. In contrast, venous and arterial forms involve blood flow. Neurogenic thoracic outlet syndrome is the common type. It makes up about 90–95% of cases. Venous thoracic outlet syndrome accounts for roughly 3–5%. Arterial thoracic outlet syndrome is rare at about 1%.
Anatomic features explain these differences. The first rib, clavicle, and scalene muscles form rigid boundaries that can compress the brachial plexus or the subclavian artery or subclavian vein. A cervical rib or abnormal first rib can push on nearby structures. Born with an extra rib is one congenital reason for narrowing. Repetitive overhead activity and trauma are other common causes. Risk factors include heavy overhead lifting, repetitive motions, and certain anatomic variants such as a cervical rib. Women in some studies present more often with NTOS, and athletes who throw or swim may also be at higher risk.
Symptoms depend on the structure affected. Nerve compression produces pain, tingle, numbness, and weakness. Venous obstruction leads to arm swelling, discoloration, and a feeling of fullness. Arterial compression may cause a change in color or coolness and may lead to arterial damage or aneurysm. Venous thrombosis can cause acute arm swelling and may require clot-dissolving therapy. Vascular surgeons and neurologists evaluate the anatomy and blood flow to decide on the best plan. For patients interested in system-level simulation of workflows and device integration, we partner with simulation tools that integrate with terminal operating systems; see our overview on simulation vs TOS for complex systems simulation vs TOS.
Drowning in a full terminal with replans, exceptions and last-minute changes?
Discover what AI-driven planning can do for your terminal
diagnosis of thoracic outlet syndrome: how we diagnose nerve and vascular compression
We begin with a focused history and physical examination. The physical examination looks for signs in the neck and shoulder and evaluates strength and sensation. We perform provocative tests to reproduce symptoms and to assess compression of the nerves or artery. The goal is to rule out rotator cuff disease, cervical radiculopathy, and other causes that mimic this condition. In practice, thoracic outlet syndrome refers to multiple presentations, so we use targeted tests to narrow the cause.
Imaging plays a central role. We use mri for soft tissue detail and ct or ct scan for bony anatomy. Ultrasound offers dynamic assessment of blood flow and is helpful when veins or arteries compress during arm positions. We also use x-ray to look for a cervical rib or abnormal first rib. Venography remains useful to map venous obstruction and thrombosis. For nerve assessment, we obtain nerve conduction studies and electromyography to quantify nerve function. Vascular surgeons and neurologists interpret these tests together.
At our center we apply a comprehensive diagnosis of thoracic outlet syndrome that integrates clinical and imaging data. We try to diagnose and treat fast when a clot threatens limb function. If imaging shows a subclavian vein clot, we act swiftly with anticoagulation and consult vascular surgeons for possible endovascular therapy. For suspected subclavian artery injury we evaluate for narrowing, dissection, or aneurysm. We also use a multidisciplinary approach and sometimes simulation tools to plan complex interventions; for operational planning and system integration examples, explore our simulation for terminal operating system decision support resource simulation for TOS decision support. Finally, we ensure each patient receives a tailored plan that may include physical and occupational therapy or referral to an appropriate surgeon for decompression surgery when needed.
neurogenic thoracic outlet syndrome (ntos): symptoms, tests and treatments
Neurogenic thoracic outlet syndrome, often shortened to ntos, affects the brachial plexus. It produces pain, tingling, numbness, and weakness in the arm and hand. Patients often describe tingle and burning sensations. They also report loss of grip strength and difficulty with fine hand tasks. Neck pain and shoulder symptoms can accompany the upper limb complaints. Because the brachial plexus contains multiple nerves, symptoms vary by the exact site and degree of compression.
Physical examination and targeted provocative tests help localize compression of the nerves. Nerve conduction and electromyography clarify which fibers show slowed conduction. These tests prove valuable when the clinical picture is unclear. Imaging with mri shows soft-tissue causes, such as scalene muscle hypertrophy or an abnormal first rib. X-ray or ct can reveal a cervical rib. An accurate diagnosis of thoracic outlet syndrome requires careful correlation of clinical and test results so we can rule out other causes.
Conservative management succeeds for many patients. We prescribe physical therapy that emphasizes posture correction and scalene stretching. We add activity modification and pain management. Physical therapy and physical and occupational therapy together restore function in the majority of cases. If conservative care fails, we may recommend surgery. Surgeons perform decompression surgery to remove the first rib or release tightened muscles. Surgical decisions follow careful assessment and only after less invasive options have been tried. Our multidisciplinary team provides follow-up rehab after surgery to regain strength and range of motion. We also work with rehabilitation specialists to avoid recurrence and to protect the spinal cord and rotator cuff during recovery.
Drowning in a full terminal with replans, exceptions and last-minute changes?
Discover what AI-driven planning can do for your terminal
venous thoracic outlet syndrome: presentation, risks and management
Venous thoracic outlet syndrome happens when the subclavian vein faces obstruction at the thoracic outlet. Patients present with sudden arm swelling, pain, and a heavy feeling. The limb may show discoloration or a change in color and may feel warm. In acute cases, thrombosis of the subclavian vein produces significant swelling and can lead to blood clots that require urgent attention. Venous thrombosis may limit function and may risk pulmonary embolism if unmanaged.
Diagnosis relies on ultrasound and venography. Ultrasound identifies clot and reduced blood flow. Venography maps the obstruction and helps plan interventions. We assess for anatomic narrowing by the first rib or clavicle and for an abnormal first rib or cervical rib that compresses the subclavian vein. In many patients, the immediate goal is to treat the clot. We use blood thinners and, when appropriate, clot-dissolving therapy. Endovascular techniques such as thrombectomy and balloon angioplasty can restore patency. If an anatomic compression remains, surgery to remove the offending rib or to perform decompression surgery may follow.
Vascular surgeons coordinate the acute and long-term plan. After clot resolution, rehabilitation focuses on restoring arm function and preventing recurrence. Patients need education on activity modification and when to seek care for new swelling. Our centre specializes in combined endovascular and surgical strategies to treat obstruction and to reduce the chance of repeat thrombosis. We also track outcomes and participate in clinical trials to evaluate new techniques for venous decompression and long-term flow preservation.

arterial thoracic outlet syndrome, clinical trials and specialize in advanced therapies
Arterial thoracic outlet syndrome involves compression of the subclavian artery and is the least common form of tos. It can produce ischemia, coolness, and weak pulses in the arm. Repeated compression may cause damage to the artery wall and lead to aneurysm or distal emboli. Patients sometimes report pain during exertion or a sudden change in color. The clinical picture can progress if a clot forms or if arterial injury produces distal embolization.
Diagnosis integrates ct imaging, duplex ultrasound, and angiography. A ct scan helps show the anatomic relationships and any abnormal first rib or clavicle that compresses the subclavian artery. Angiography clarifies arterial narrowing. If arterial damage exists, vascular surgeons may recommend surgery to remove the compression and to repair or bypass the affected segment. Surgery to remove the first rib or to correct an abnormal bone often restores blood flow. In some cases, grafts or arterial reconstruction become necessary to protect blood flow and to prevent further embolic events.
Clinical trials are testing less invasive decompression techniques and optimized pathways for combined vascular and orthopaedic care. We participate in clinical trials and in quality registries to expand evidence for surgical timing and for endovascular adjuncts. Our centre specialize in tailored surgical and rehab pathways. We assemble a team of vascular surgeons, physiotherapists, and occupational therapists to plan care from diagnosis through recovery. We pair surgical expertise with structured rehabilitation to regain function while minimizing recurrence. For teams that manage complex systems and need TOS-agnostic integration with simulation, Loadmaster.ai shows how agents can integrate across operating systems and still adapt to changing constraints TOS simulation tools. We follow evidence and offer expert care that aims to restore blood flow and limb function with the least delay.
FAQ
What exactly is thoracic outlet syndrome?
Thoracic outlet syndrome is a group of conditions caused by compression at the outlet between the neck and upper chest. Symptoms arise when nerves or blood vessels compress and include pain, weakness, and sensory changes.
What are the main types of thoracic outlet syndrome?
The three primary types are neurogenic, venous thoracic outlet syndrome, and arterial thoracic outlet syndrome. Neurogenic is the common type, while venous and arterial forms are less frequent.
How do you diagnose thoracic outlet syndrome?
Diagnosis combines a focused physical examination with imaging such as mri, ct, ultrasound, and sometimes venography. We also use nerve conduction studies to evaluate nerve function and to rule out other causes.
What symptoms suggest neurogenic thoracic outlet syndrome?
Neurogenic thoracic outlet syndrome produces pain, tingle, numbness, and weakness in the arm and hand. Patients often notice worsened symptoms with certain arm positions.
When is surgery recommended?
We may recommend surgery when conservative measures fail or when vascular injury, thrombosis, or arterial damage threatens limb function. The decision follows a comprehensive diagnosis and multidisciplinary review.
What treatments exist for venous problems?
Acute venous thrombosis often requires blood thinners and sometimes clot-dissolving treatment or endovascular thrombectomy. If anatomic compression remains, decompression surgery to remove the first rib may prevent recurrence.
Are there non-surgical options?
Yes. Physical therapy, posture correction, and activity modification help many patients. Physical therapy and physical and occupational therapy are core parts of initial care.
Can a cervical rib cause thoracic outlet syndrome?
Yes. A cervical rib or an abnormal first rib can compress nerves or blood vessels and cause symptoms. Surgical removal of an extra rib may be necessary in some cases.
How urgent is treatment for arterial involvement?
Arterial involvement can be urgent because it threatens blood flow and risks embolism or aneurysm formation. Rapid evaluation with ct scan and vascular specialist input is important.
Do you offer multidisciplinary care?
Yes. We provide multidisciplinary assessment that includes vascular surgeons, neurologists, and rehabilitation specialists. This team approach helps diagnose and treat patients efficiently and safely.
our products
 stowAI
stowAI
 stackAI
stackAI
 jobAI
jobAI
Innovates vessel planning. Faster rotation time of ships, increased flexibility towards shipping lines and customers.
Build the stack in the most efficient way. Increase moves per hour by reducing shifters and increase crane efficiency.
Get the most out of your equipment. Increase moves per hour by minimising waste and delays.
 stowAI
stowAI
Innovates vessel planning. Faster rotation time of ships, increased flexibility towards shipping lines and customers.
 stackAI
stackAI
Build the stack in the most efficient way. Increase moves per hour by reducing shifters and increase crane efficiency.
 jobAI
jobAI
Get the most out of your equipment. Increase moves per hour by minimising waste and delays.
